Sometimes, reading your patient portal to get your test results or doctors’ notes is like reading a foreign language. The information you find may be difficult to decipher because your care team uses words, abbreviations and terminology you likely haven’t encountered in the past.
Patient portals are an important tool designed to help facilitate effective and efficient communication between you and your care team, as well as between your health care providers. A 2019 study of cancer patients and their use of patient portals published in the Journal of Cancer Treatment and Diagnosis found that:
- 65 percent of patients said having the ability to access their personal health record through a patient portal helped them better communicate with their physicians.
- 83 percent said they learned new and useful information through their portal.
But the usefulness of that health information is enhanced when you understand at least some of the terminology. Otherwise, as the study noted, patients may experience “heightened anxiety and confusion.”
A 2021 study in Cancer Medicine, however, concluded: “When patients with cancer have access to portals, they feel more informed and more in control of their disease and also feel in better control of their treatment.”
"When a patient first comes into the room, I usually ask them, 'Tell me your understanding of things that are going on,'” says Cynthia Lynch, MD, Medical Oncologist at City of Hope Phoenix. “I want to hear their words, the terminology they’re using, so I can best meet them where they are and take them to the next level of understanding."
This article is designed to help you navigate some of the common cancer terms you may encounter when browsing your record in the patient portal, helping you develop a better understanding when you speak to your cancer care team members. Topics include:
- The ’omas: Carcinoma, sarcoma and more
- Cancer diagnosis terms: Poorly differentiated, apoptosis and more
- Cancer treatment terms: Unresectable, precision medicine and more
- Where to learn more
If you’ve been diagnosed with cancer and are interested in a second opinion on your diagnosis and treatment plan, call us or chat online with a member of our team.
The ’omas: Carcinoma, sarcoma and more
If you’re familiar with Greek or Latin—the origins of many medical terms—you may be able to dissect cancer-related words. For instance, the prefix "onco" has origins in Greek (onkos, meaning growth or lump) and Latin (onco, meaning tumor). Those are the roots of the word oncology, meaning the study of cancer; oncologists, the name for doctors who treat cancer; and oncogenes, which are genes with the potential to mutate and help cancer cells develop.
A word ending in “oma,” a suffix believed to be used first by the ancient Greek physician Galen, often ends a word that denotes a type of cancer. Below are some examples, including words that describe cancers and other conditions.
Adenocarcinoma: This type of cancer forms in the glandular tissue lining internal organs, which produce fluids like mucus and digestive juices. Most cancers of the breast, lung, esophagus, stomach, colon, rectum, pancreas, prostate and uterus are adenocarcinomas.
Carcinoma: This is the most common form of cancer. It usually forms in skin cells or in the lining of organs, such as the kidney or liver.
Fibroma: This is usually a non-cancerous uterine fibroid.
Glioblastoma: This is the most common and aggressive form of brain cancer.
Hemangioma: This common type of birthmark, made up of extra blood vessels in the skin, is a benign (non-cancerous) growth.
Hematoma: This pool of blood forms in an organ, tissue or body space, usually due to a blood vessel broken through surgery or an injury. Most hematomas are small and go away on their own, but some may need to be surgically removed.
Lipoma: This benign—non-cancerous—tumor is made of fat cells.
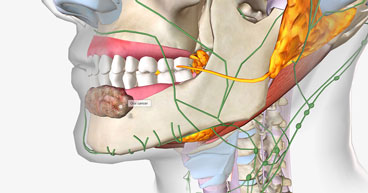
Lymphoma: This cancer begins in cells of the immune system or lymphatic system, which is made up of a network of lymph vessels and nodes that help the body fight infections. The two basic categories of lymphomas are listed below.
- Non-Hodgkin lymphoma, the more common of the two, is classified by more than 30 types, characterized by the type of cell involved.
- Hodgkin lymphoma, which used to be known as Hodgkin’s disease, is a rare cancer with fewer than 9,000 cases diagnosed each year, according to the American Cancer Society (ACS).
Melanoma: This cancer develops in melanocytes, the skin cells that produce melanin, which give skin its color.
Myeloma: This cancer forms in plasma cells, a type of white blood cell.
Neuroblastoma: This type of cancer forms from immature nerve cells and is most often diagnosed in children under age 5.
Retinoblastoma: This cancer forms in the tissues of the retina, or the light-sensitive nerves at the back of the eye, and usually is diagnosed in children.
Sarcoma: This rare form of cancer usually grows in the body’s connective tissue cells like fat, blood vessels, nerves, bones, muscle and cartilage.

Cancer diagnosis terms: Poorly differentiated, apoptosis and more
If you’re reviewing your lab results, pathology reports or provider’s notes, understanding definitions of common terms may go a long way in helping you decipher the report and formulate your questions before you have a conversation with your physician.
Some common diagnostic terms include those below.
Abnormal or atypical: These may be self-explanatory, but an abnormal or atypical lesion or growth anywhere in or on the body may not be cancerous. It may be benign (non-cancerous), precancerous or premalignant (likely to become cancer if not treated) or malignant (cancerous).
Angiogenesis: This process of developing new blood vessels is a vital step in the development of tumors. Among targeted therapy drugs used to treat cancer are angiogenesis inhibitors, designed to prevent tumors from developing new blood supplies.
Apoptosis: In this process, old or damaged cells die off in order to make room for new cells. Cancer cells evade apoptosis and grow unchecked when untreated or when treatment fails.
Benign tumor: This growth is not cancer and will not likely spread to nearby tissue.
In situ: This is Latin for “in its original place.” With a carcinoma in situ, abnormal cells are found only in the place where they first formed and have not spread.
Indolent cancer: This cancer grows very slowly.
Leukopenia: This condition is marked by a low number of white blood cells in the bloodstream.
Lymphatic system: This network of vein-like vessels throughout the body carries a watery fluid called lymph, which delivers oxygen and nutrients to cells and carries away cellular waste products.
Malignant: This term is used to describe cancer cells that grow in an uncontrolled way, invading nearby tissues and spreading to other parts of the body through the blood and lymph system.
Metastasis: This term is used to describe cancer that has spread to another part of the body.
Mutation: This is when a cell undergoes a permanent change to its DNA. All cancers are a result of gene mutations, which can be inherited, due to aging or exposure to toxins or substances like cigarette smoke.
NEOD/NED: An abbreviation meaning “no evidence of disease.”
Poorly differentiated, undifferentiated, well differentiated: Used to help determine a cancer’s grade, these describe how the cells of the tumor look under a microscope.
- Poorly differentiated or undifferentiated cells are abnormal cells without well-formed structures. These types of cells often grow and spread quickly and correspond to a high-grade cancer or tumor, which may require immediate, possibly aggressive, treatment and may have a poor prognosis.
- Well-differentiated cells are associated with a low-grade cancer or tumor, which may not grow as rapidly.
Prognosis: The likely or predicted outcome over the course of a disease as well as the likelihood of recovery or recurrence.
Remission: A decrease in or disappearance of signs and symptoms of cancer. In partial remission, some, but not all, signs and symptoms of cancer have disappeared. In complete remission, all signs and symptoms of cancer have disappeared, although cancer still may be undetected in the body.
Neoplasm: Another word for tumor or mass of tissue due to excessive cell growth. The growth may be cancerous or benign.
Node negative: The cancer has not spread to the lymph nodes or part of the lymphatic system.
Stage: Assigned to a cancer—0 through 4—when it’s diagnosed to signify how advanced the cancer is. The lower the stage, the better the prognosis, with stage 4, meaning the cancer has spread to other areas of the body.
Tumor grade: Associated with the type of cancer cells—poorly differentiated, undifferentiated or well differentiated—with a higher grade meaning the cells will likely grow and spread more quickly.
Cancer treatment terms: Unresectable, precision medicine and more
When considering your treatment options, it helps to know a few key terms you may see in your personal health record in the patient portal. They’ll also be useful in discussions with your care team.
Ablation: This is the removal or destruction of tissue or a body part through surgery, hormones, drugs or other methods.
Adjuvant/neoadjuvant therapy: This treatment is used in combination with another treatment. A primary or first-line therapy like surgery or radiation therapy may be preceded by or followed with another therapy like chemotherapy, immunotherapy, targeted therapy or hormone therapy. Treatments given before the primary therapy are called neoadjuvant, while those delivered after the primary therapy are termed adjuvant therapies.
Chimeric antigen receptor T-cell or CAR T-cell therapy: In this therapy, T-cells are removed from the patient’s bloodstream, reprogrammed to attack the patient’s cancer, then delivered back into the bloodstream.
Checkpoint inhibitors: This is a type of immunotherapy designed to interrupt the signals that allow cancer cells to hide from the body’s immune system.
Chemotherapy: This is among the most common and often a first-line treatment that uses drugs to kill cancer cells or stop their growth. The drugs may be given orally, by injection or infusion, or on the skin.
Dysplasia: This refers to abnormal cells that precede the development of full-blown cancer.
Endocrine or hormone therapy: This type of treatment is used to treat cancers like breast and prostate cancer that depend on bodily hormones to grow. These treatments are designed to block the body’s ability to produce hormones.
Genetics or genomics: These terms often are used interchangeably because both involve the study of genetic material, these terms have very different meanings.
- Genetics is the study of the genes people inherit from their family through generations.
- Genomics is the study of mutations in tumors themselves that may explain how the cancer behaves.
Mapping a person’s genetic profile, as well as analyzing a tumor’s genomic abnormalities, may help doctors determine what’s driving the cancer’s growth and target treatments for those specific features.
Immunotherapy: Sometimes known as biologic therapy, these drugs are designed to stimulate the immune system or help it better recognize and attack cancer cells.
Lymphedema: This occurs when extra lymph fluid builds up in tissues and causes swelling usually due to lymph vessels that are blocked or damaged or that have been surgically removed.
Resectable: This term is used to describe cancerous tissue that may be removed surgically. Unresectable means it cannot be removed by surgery.
Margin: This is the perimeter of normal tissue that surrounds cancer cells or a tumor that is removed during cancer surgery. If cancerous cells are found in the margin after a pathology lab analysis, it may mean another surgery is necessary in order to achieve a “negative margin” or tissue free of cancerous cells.
Off-label: This refers to the practice of prescribing a drug to be used in a way not outlined on its label or as approved by the FDA.
Palliative treatment: This is care that, rather than treating a disease, is designed to improve quality of life, including reducing pain and treating the symptoms of cancer. It’s different from hospice care, which is end-of-life care when all treatment has ended and only comfort care is provided.
Precision medicine: These treatments use information from an individual’s genetic profile or a tumor’s genomic profile to diagnose or treat disease. Precision medicine uses information from these profiles to better target specific features on an individual’s cancer.
Radiation therapy: This common treatment uses radiation from X-rays, gamma rays, neutrons and protons from external machines as well as radioactive material placed inside the body to kill cancer cells and shrink tumors.
Reconstructive surgery: These special surgical procedures are designed to rebuild a body part affected changed by a previous operation. This approach may also be used to reconstruct parts of the body disfigured by the cancer itself.
Targeted therapy: This treatment uses information from genetic, genomic or lab tests to target specific molecules that allow cancer cells to grow.
Tumor-agnostic or tissue-agnostic therapy: This is a therapy used for multiple cancer types that targets specific genomic mutations, no matter where in the body the cancer originated.
Where to learn more
These terms are just a few of the dozens you may encounter as you peruse your patient portal. The websites for the National Cancer Institute and the ACS have comprehensive glossaries of cancer terms that you may find useful.
But the most useful source of information about your diagnosis, prognosis or treatment is your care team. They can help you navigate the terminology that pertains to your situation, and they often understand that you may not speak their language of medical terminology.
"Don't spend a lot of time stressing and searching for answers,” Dr. Lynch says. “Make sure you have a provider you’re comfortable with and can ask questions of. Reach out to your doctor, because a lot of times, things can be cleared up quickly."
If you’ve been diagnosed with cancer and are interested in a second opinion on your diagnosis and treatment plan, call us or chat online with a member of our team.