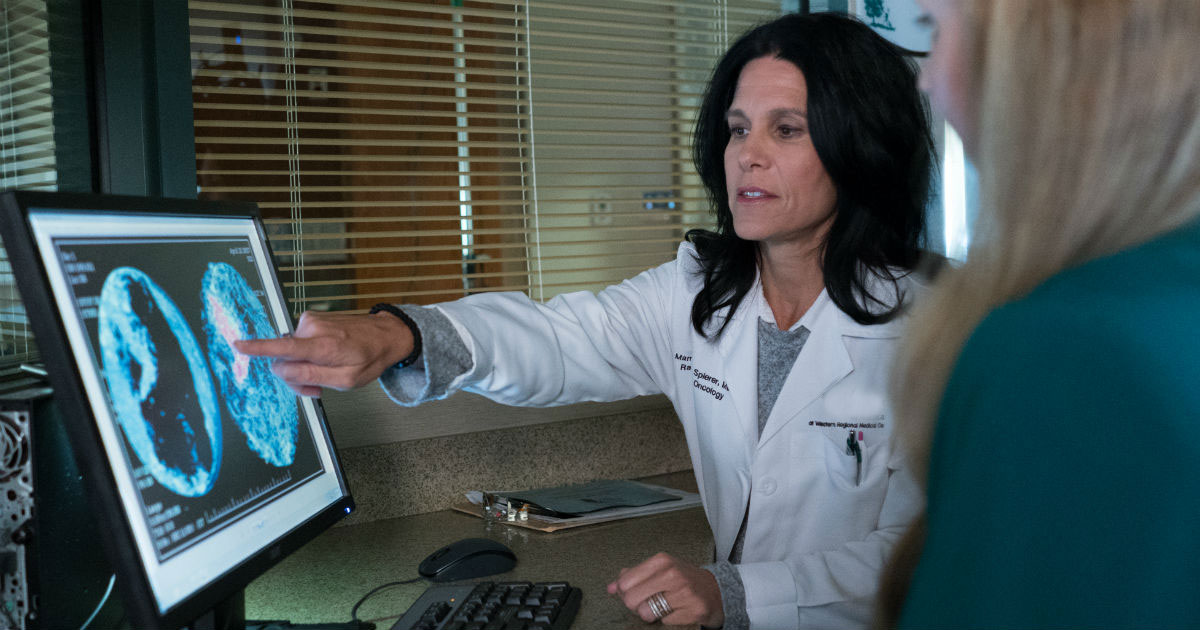
Imaging tests are a way for doctors to help see inside the body when they suspect something might be wrong, such as bone fractures, lung disease or a tumor. These tests work by using forms of energy—like an X-ray or magnetic field—to generate images.
Thanks to advances in technology, doctors today have a multitude of imaging procedures to help diagnose and stage disease—and determine which treatments will be most effective. Still, for many patients, it may feel a bit like alphabet soup when they hear their doctor throw around terms like:
- Computed tomography (CT) scan
- Magnetic resonance imaging (MRI)
- Positron emission tomography (PET) scan
Patients may feel especially confused when their doctor recommends one over the other.
In this article, we’ll explore the differences between imaging tests and the factors doctors consider when determining which may be appropriate for you. We’ll look at:
- MRI vs. CT scan
- Scans with contrast
- How to prepare for a CT scan
- How to prepare for an MRI
- What is a PET scan?
- What is an ultrasound?
If you’re interested in getting screened for cancer or if you’ve been diagnosed with cancer and want a second opinion, call us or chat online with a member of our team.
MRI vs. CT scan
MR and CT scans are two of the most common imaging tests used to diagnose and stage cancer and to assess the response to cancer treatments. And they may often be conflated.
So, what’s the difference? Plenty.
- CT scans use radiation, MRI scans don’t.
- MRIs generally cost more, up to twice as much of a CT scan.
- CT scans are faster. In fact, with the technology available today, radiologists and radiology technologists can scan someone from head to foot in less than 30 seconds. An MRI could take 30 minutes or longer.
- MRIs are noisy and may require patients wear earplugs or headphones. CT scans are pretty quiet.
- CT scans use a narrow ring, while an MRI may require patients to spend extended time in a tube.
A CT scan aims a narrow beam of X-rays at a patient and rotates the beam around the body. The reconstructed X-rays produce thin, cross-sectional images, or slices. These images are then stacked to form a 3D image. CT scans can show a tumor’s location, shape and size, and may be very helpful with cancer staging.
“You can think of it as a very fancy X-ray,” says Jason Beland, MD, Chair of the Department of Radiology at City of Hope Atlanta, Chicago and Phoenix and Medical Director of Imaging Services at City of Hope Atlanta. “CT scans take advantage of different densities, such as muscles, organs or bones. They’re much more sensitive than a regular X-ray and can show abnormalities much more clearly.”
On the other hand, an MRI uses a large magnet and computer-generated radio waves to create detailed images.
“If the strength of CT is its spatial resolution, the strength of MRI is its tissue contrast,” Dr. Beland says. “It has the ability to show abnormalities in the tissue itself.”
If you hurt your knee, for example, your doctor would likely recommend an MRI to take a close look at the muscles, tendons and ligaments in your knee. As it relates to cancer, MRI is generally superior to a CT scan when it comes to imaging organs in the body like the brain and the liver. That’s because it can differentiate normal tissue with abnormal tissue, making lesions easier to see.
Still, when performing routine imaging of the body—chest, abdomen and pelvis—in a patient with cancer, “CT is the workhorse,” Dr. Beland says, “because we can scan very quickly and get a good sense of where disease is in the body. It’s fast and it can tell us the status of disease and whether lesions are new, bigger or smaller.”
CT scans are very useful for diagnosing and staging cancer, checking to see if cancer has returned and monitoring whether treatment is working. It’s also useful to see if cancer has spread, or metastasized.
“There are reasons why we choose one test over another, and there are usually tradeoffs, but we choose the best test for the specific questions we’re looking to answer,” Dr. Beland says. “It’s usually not about getting a specific test because of what you have.”

Dr. Jason Beland
Scans with contrast
Contrast dyes are often used with MRI and CT scans to better highlight different tissue. They contain materials like barium, iodine and gadolinium, and can be given orally or intravenously (through the vein). Most often, the dye is injected into the blood, travels through the arteries and veins, and often highlights the differences between normal tissue and diseased tissue.
Contrasts are different for each type of scan, Dr. Beland says. For instance, if you have an MRI, you’ll typically get 10 to 20 milliliters of contrast injected, while in a CT scan, you’ll get 50 to 100 milliliters.
Potential side effects of a CT contrast include an allergic reaction and slight risk of kidney damage. With MRI contrast, on the other hand, “You’re less likely to be allergic, it’s lower volume and it’s safer for kidneys,” Dr. Beland says.
How to prepare for a CT scan
Although all imaging tests are painless, there may be some preparation involved with each.
Because the contrast is cleared by the kidneys, you’ll have to undergo bloodwork before getting a scan with contrast to make sure your kidneys are working as they should.
Also, before both a CT and MRI scan, patients are asked not to eat. That’s because the contrast can sometimes make people nauseous.
If you receive oral contrast, you’ll likely need to start drinking the solution an hour or two before your scan. If contrast is given intravenously, a catheter will be inserted into your vein, or an existing access line, which many cancer patients already have.
How to prepare for an MRI
With MRI, it’s important to prepare for a lengthier test during which you have to remain completely still. That can be hard for patients who are sick, have back pain or claustrophobia.
Sometimes, medicine may be necessary to ease discomfort or split the exam into separate sections. Alternatively, MRI might not be the best test for someone who can’t hold still. “If you end up with blurry pictures,” Dr. Beland says, “the advantages of an MRI are moot.”
Doctors can use information from a CT scan to help better tailor the MRI, though. For example, if they see on a CT scan that the disease is in the middle of the spine, they may order an MRI of the thoracic spine instead of the whole spine to shorten the length of the test.
When preparing for an MRI, it’s also vital to remember that the machine is a strong magnet, which means that it can move things that are ferromagnetic (meaning they’ll stick to the magnet), including metal shrapnel, implants or devices. Having these implanted metals may distort images on MRI scans. The powerful magnet may damage batteries in implanted devices, such as pacemakers, pumps or defibrillators, but also your phone, watch and even magnetic strips on credit cards.
Another important note with MRI is that the magnet can cause metal to heat up. “These are the things we have to pay attention to,” Dr. Beland says.
What is a PET scan?
Another type of commonly used imaging test in oncology is a PET scan, which is a noninvasive nuclear imaging test that uses a radioactive drug, called a tracer, to show areas where cancer may have spread. The radioactive drug collects more in specific types of cells helping show the location of certain cancer types.
A PET scan is most often referred to as a PET/CT, because the information from the PET is overlayed with a non-contrast CT scan to provide better anatomic detail and the location a tumor.
What is an ultrasound?
Ultrasound is another frequently ordered imaging test. Like MRI, it doesn’t use radiation. Instead, it captures images of soft tissue structures inside the body with high-frequency sound waves. A handheld device called a transducer sends and receives ultrasound signals.
This type of test is best to evaluate specific tissues, such as the breast, gallbladder, kidneys or uterus. It takes advantage of the speed of sound through tissue and can differentiate between solid and cystic structures.
Whichever test your doctor orders, you can be sure it’s personalized to your unique diagnosis, needs and treatment goals.
“No test is better than the others,” Dr. Beland says. “They’re all good, just in different ways.”
If you’re interested in getting screened for cancer or if you’ve been diagnosed with cancer and want a second opinion, call us or chat online with a member of our team.



