Humans are not robots, but our minds and bodies are programmed so that most of us can perform many normal tasks with machine-like efficiency, even without thinking about them. Cancer and its treatments, however, often rob patients of senses, movements or bodily functions that once come naturally. Surgery may make some movements more painful, for instance. Chemotherapy may affect the patient’s cognitive abilities, hearing and digestive function.
For patients with head and neck cancers, cancer symptoms and treatment side effects often complicate two innate tasks that are usually taken for granted—speaking and swallowing. Thanks to modern medicine, though, new-generation therapies and special devices have helped some patients regain their abilities, says Jennifer Cargile, MEd, Speech-Language Pathologist at Cancer Treatment centers of America® (CTCA), Atlanta.
“The top concerns I hear are, ‘How am I going to be able to communicate with the world?’” she says. “And, ‘Hold on, what do you mean I might not be able to eat like I currently do?’ I tell them, it’s ok. You’ll just do these things differently.”
In this article we’ll review:
- Head and neck cancer treatments and side effects
- Types of head and neck surgeries
- Voice restoration options:
- A case study: How Val Kilmer regained his ability to speak
- Head and neck cancer treatment at CTCA®
If you’ve been diagnosed with a head and neck cancer and want to explore your treatment options, or if you’re interested in a second opinion on your diagnosis and treatment plan, call us or chat online with a member of our team.
Head and neck cancer treatments and side effects
Treatments options for head and neck cancers often include radiation therapy, surgery and chemotherapy. For patients with laryngeal cancer specifically, these treatments may produce challenging side effects that may make it difficult to speak or swallow or indirectly affect a patient’s ability to eat.
Radiation therapy
The vocal cords are made of two slim strands of tissue located in the larynx, which is often called the voice box. The cords vibrate as air passes through them, producing sounds. Vocal cords also help regulate airflow in and out of the lungs and help prevent food and saliva from seeping into the airways.
Radiation therapy may damage the cords and stiffen the strands of tissue. As a result:
- They may not be able to close properly to protect the airways.
- Stiffness in the cords may produce a hoarse or raspy voice.
- Patients may have difficulty swallowing.
Some patients are able to adapt to these side effects, Cargile says. But others may later decide, in consultation with their care team, to opt for surgery.
“Some patients are OK with a raspy voice, and they continue to be able swallow after radiation treatment. That’s a win-win,” Cargile says. “But I’ve also had patients who are raspy and they couldn’t swallow, and who’ll then say, ‘This is not what I signed up for.’”
Surgery
Doctors may recommend surgery to remove tumors or other cancerous tissue. Plastic surgeons may also rebuild some features to improve the patient’s physical appearance and/or restore function. The National Cancer Institute recommends several surgical options to treat head and neck cancers, including:
Cordectomy: This surgery is performed to remove one or both vocal cords. The patient’s ability to speak will depend on how much of the vocal fold tissue is removed.
Supraglottic laryngectomy: This surgery is performed to remove just the supraglottis, which is located just above the vocal cords in the larynx. The patient may be able to retain a normal speaking voice after the procedure.
Hemilaryngectomy: This surgery is performed to remove half the larynx or one vocal cord. This option saves the voice, but speech tends to be more limited.
Partial laryngectomy: This surgery is performed to remove only the cancerous part of the larynx to keep as much of the organ intact as possible.
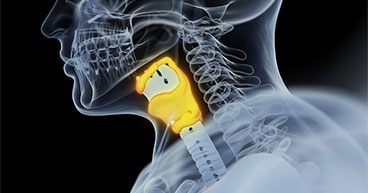
Total laryngectomy: This surgery is performed to remove the whole larynx. During this operation, the surgeon creates a hole in the front of the neck to allow the patient to breathe. This procedure is called a tracheostomy, and the hole through which the patient will breathe is called a stoma. The patient will not be able to speak as he or she did before the surgery but can learn to speak in other ways.
Chemotherapy
These drugs may not affect the patient’s ability to speak or swallow, but they may make it more difficult to eat. Common side effects of chemotherapy include:
- Mouth sores
- Metallic taste
- Digestive issues
Immunotherapy and targeted therapy may also be recommended for some head and neck cancers.
Voice restoration options
Three basic elements are needed to make it possible to speak:
- A power source, typically air from the lungs
- A sound source, typically the vocal cords in the larynx
- A sound modifier to form words, which usually occurs in the pharynx or the area behind the nose and mouth as well as the tongue and mouth cavity
How each of these elements functions after head and neck cancer treatment may help determine the therapy or device necessary to help patients regain the ability to speak and swallow.
When the larynx has been removed in a total laryngectomy, the sound source is no longer available. The surgery also disconnects the lungs from the vocal tract, so the power source no longer generates air from the lungs into the larynx. Instead, the stoma serves as the power source of air, enabling speech.
“After a total laryngectomy, you will always breathe through your neck,” Cargile says. “That means, if you need CPR, rescue personnel would put the oxygen source over your neck, directing the oxygen into your stoma. If you’re taking a shower, you’d have to be careful not let water penetrate the stoma because it would go straight into your lungs.”
Esophageal speech
This is a low-tech, no-cost option, but it requires mastering a technique in which the patient gulps air into the esophagus and then up into the throat, using the mouth to form words as the air escapes.
“I have a few patients who know how to do it,” Cargile says. “But they say it’s tiresome to sit there and have to do it over and over again, and they can only get so many words out per air flow.”
Electrolarnyx
This is an external device attached to the front or side of the throat that acts as the vibrating sound source for speech. These devices are relatively inexpensive, and they’re not too difficult to learn how to use, especially when working with a speech therapist.
One disadvantage to an electrolarnyx is that it produces a mechanical, buzzy tone that doesn’t vary like natural speech does. While this device may preserve certain speech patterns and even regional accents, the voice quality will not be the same as it was before the surgery.
Tracheoesophageal puncture
This increasingly popular voice restoration option uses a prosthetic valve that allows a person to speak. The valve is inserted into the channel between the windpipe and esophagus in a procedure called a tracheoesophageal puncture (TEP). The surgeon may perform a TEP as part of a laryngectomy or at a later date.
To speak, the patient exhales, allowing air to pass over the valve and providing a new sound source. The valve only opens in one direction, preventing food and fluids from going down the esophagus.
This option produces more natural sounds than an electrolarynx, but it’s more expensive and needs careful maintenance and cleaning. The valve costs about $300 and needs to be replaced every 60 days to six months.
Even with proper cleaning, the valve wears down over time and may even start leaking, increasing the risk of aspirating food or fluid getting into the lungs. But speech therapists are able to replace worn valves in a quick, relatively painless procedure, Cargile adds.
Val Kilmer speaks again
Actor Val Kilmer is a prominent example of someone who successfully regained his voice after treatment for throat cancer. And his case offers a glimpse into the potential future of voice restoration for head and neck cancer patients.
Kilmer was diagnosed in 2015 and, as a result of treatment, the star of hit movies Top Gun and Tombstone lost his ability to speak.
Today, thanks to therapy and promising new artificial intelligence (AI) technology, Kilmer speaks again in a voice very much as it used to be. The technology uses a vocal library of words Kilmer speaks in his various movies and public interviews to digitally reproduce his voice.
“After getting treated, my voice as I knew it was taken away from me,” Kilmer’s says with is reconstructed voice. “People around me struggle to understand me when I’m talking. But despite all that, I still feel I’m the exact same person. Still the same creative soul. A soul that dreams ideas and stories constantly. But now I can express myself again. I can bring these dreams to you and show you this part of myself once more. A part that was never truly gone, just hiding away.”
Kilmer chronicled his recovery from throat cancer over the past six years in a 2021 Amazon Prime documentary.
High tech devices using artificial intelligence like the one used by Kilmer are still under development, but some seem promising. For instance, in a 2019 study detailed in the journal Head and Neck, researchers used sensors on a patient’s face and neck that recognized words silently mouthed and recreates them aloud.
Head and neck cancer treatment at CTCA
At CTCA, we treat head and neck cancers with a range of techniques and technologies and treatment options. CTCA’s whole-patient approach also means your team may include a speech therapist, like Cargile, who can advise you on the potential impact of each treatment option, offer therapeutic exercises and teach you to use voice restoration devices.
These experts may also be able to offer guidance on exercises to help patients address swallowing issues, that may be a treatment side effect. They are there to help educate and train you to communicate and join family and friends for meals with confidence once again.
Regardless of the therapy, exercise or device used to help regain communication or swallowing ability after treatment for head and neck cancer, a positive approach often is key to producing better outcomes, Cargile says.
“Patients say: ‘I wish I’d never taken any of this for granted — to eat or sit down and have a conversation with a loved one,” says Cargile. “I tell patients that their mindset has a lot to do with their success rate. Working with patients allows me to give them back something they had lost. That is so fulfilling.”
If you’ve been diagnosed with a head and neck cancer and want to explore your treatment options, or if you’re interested in a second opinion on your diagnosis and treatment plan, call us or chat online with a member of our team.