As a new wave of COVID-19 cases surges across the nation, hospitals in some regions are at or near capacity. Health care workers are stressed, and supplies of personal protective equipment (PPE)—masks, gowns and shields—are in short supply in some areas.
To help relieve the pressure and free up resources, public health agencies, the U.S. Centers for Disease Control and Prevention the U.S. Centers for Medicaid and Medicare Services and other public health agencies have recommended that some hospitals postpone or suspend elective surgeries and other procedures not considered immediately necessary. Doing so may help open more hospital rooms, surgical suites, help free hospital staff and equipment for the growing number of COVID-19 patients and others with serious diseases, including cancer. It may also help reduce the risk of exposure by reducing the number of people in the hospital.
So, what’s considered an elective procedure? Defining what qualifies isn’t always easy. But when it comes to cancer, it’s important for patients to know that few procedures are considered optional. “Cancer care is not elective,” says Julian Schink, MD, Chief Medical Officer for Cancer Treatment Centers of America® (CTCA). “End of story.”
What is considered elective?
Surgeries and other procedures may be considered elective if:
- They are performed by choice, not because of a serious illness or condition.
- They are related to a condition and may be beneficial or necessary, but do not need to be performed immediately.
But what is considered elective for one person may be necessary for another. For instance, if a patient is choosing to get nose surgery (rhinoplasty) to change its size or shape for cosmetic reasons, that would likely be considered elective. If a patient is scheduled for nose reconstruction to correct breathing issues and scarring caused by a head and neck cancer, that may be considered non-elective or necessary.
During the pandemic, a procedure may be considered elective depending on the region of the country. In areas where COVID-19 is surging and hospitals are at or near capacity, all non-emergency surgeries or procedures may be considered elective. In other areas, where the pandemic is less urgent, resources may be more available to perform elective procedures.
The type of hospital or health care setting involved may also be a factor. Many general hospitals—those that see patients with all types of diseases, ailments and medical emergencies—are strained to capacity because of COVID-19, forcing surgeries, diagnostic tests and screenings to be postponed. Hospitals that focus on specific illnesses, such as cancer, may not have the same restrictions. For instance, after a mastectomy is performed to treat breast cancer, a breast reconstruction procedure may be delayed at some general hospitals but performed at a cancer center without diverting resources away from COVID-19 patients.
“COVID is a new normal,” Dr. Schink says. “We have learned how to take care of patients in the era of COVID in a way that reduces the risk to the point where we can continue to deliver cancer care.”
Arthur Caplan, PhD, professor of bioethics at New York University, told The ASCO Post that it’s critical for doctors to better define essential health services in field such as cancer care, so that patients get the treatments they need. Dr. Caplan uses three criteria to define essential health care services:
- Is the procedure lifesaving?
- Does it restore function and improve quality of life?
- Can it be performed safely?
“We know that COVID has done grave damage to cancer care in the United States and in other countries,” he told The Post. “We’ve been in a situation whereby pushing all sorts of resources to COVID, … we didn’t really think through a way to prioritize services.”
Diagnostics and screenings
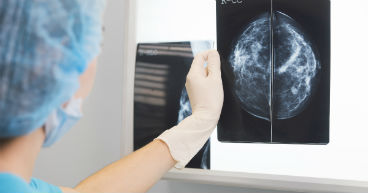
The COVID-19 pandemic is not only delaying treatments and procedures for those who are sick, it may be impacting those who don’t even know they’re sick yet or affecting others living with symptoms that need a doctor’s attention. According to an American Society of Clinical Oncology (ASCO) survey, about two-thirds of Americans scheduled for cancer screenings, such as a colonoscopy or mammogram, had their procedure postponed between July and September 2020 because of the pandemic. There also have been sharp declines in the number of new cancer diagnoses since the pandemic’s early days.
“When you consider cancer screenings, is a PSA (prostate specific antigen) test elective? Is a mammogram elective?” Dr. Schink asks. “I don’t think a patient getting those procedures would consider them elective. I consider that part of your cancer treatment.”
The delays in screenings and diagnostic tests have experts fearing a surge of new cancer cases in the coming years. Some estimate we may see as many as 10,000 additional deaths from colorectal and breast cancers in the next 10 years, due to delayed diagnostics and treatments.
Dr. Schink urges patients to talk to their doctor sooner rather than later about scheduled screening procedures and to address symptoms they may be having.
“Cancer doesn’t wait,” he says. “Don’t wait if you’re having pain or having symptoms or something points to the potential of cancer, your diagnostic procedure shouldn’t wait.”
Learn what cancer patients should know about COVID-19 vaccines.