

This page was reviewed under our medical and editorial policy by
Maurie Markman, MD, President, Medicine & Science
This page was updated on May 27, 2022.
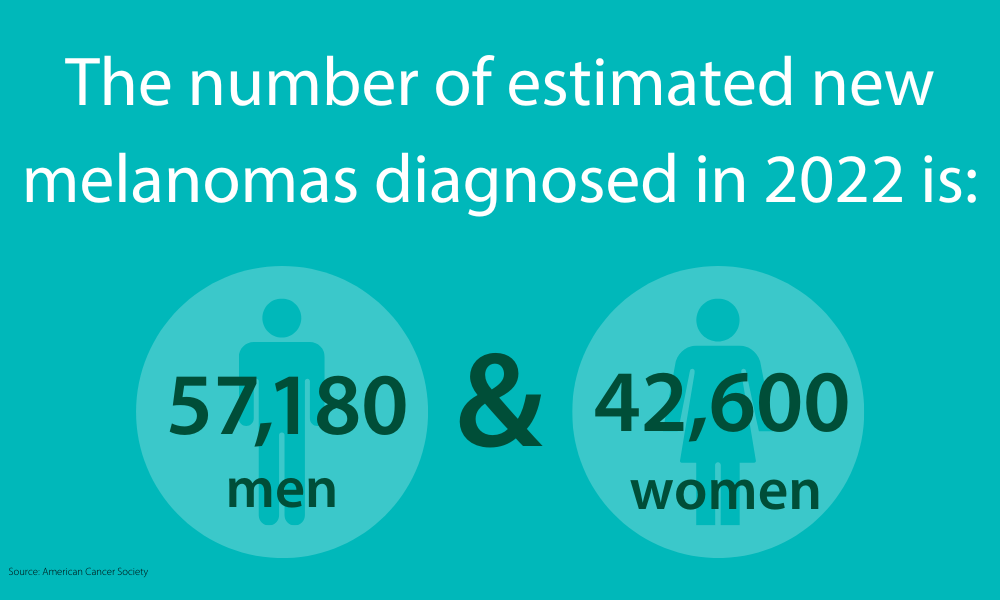
In 2025, approximately 104,960 people will be diagnosed with melanoma, and about 8,430 melanoma patients will die of the disease.
The Melanoma Research Foundation and the American Cancer Society (ASC) recommend monthly self-examinations and annual doctor visits to screen for potential skin cancer, but only a doctor can determine whether a suspicious spot or mole is melanoma.
Some tests designed for diagnosing melanoma include:
Your doctor may remove the suspicious growth, or a piece of it, for examination by a laboratory, where the pathologist will inspect the sample for cancerous cells.
Various biopsy methods are used in diagnosing skin cancers.
Melanoma biopsies can be excisional or incisional. An excisional biopsy takes off the entire lesion along with a small margin of normal skin around it, while an incisional biopsy removes only part of a suspicious lesion.
Skin biopsy: If your dermatologist notices a suspicious-looking mole, a skin biopsy is usually warranted. Your doctor will remove as much of the suspicious area as possible and send it to a lab for analysis. It’s worth noting this procedure can leave a scar.
Shave (tangential) biopsy: A shave biopsy involves removing or shaving off the top layers of the skin with a small blade. Because this type of biopsy doesn’t remove deep layers of tissue, it’s an option when your melanoma risk is thought to be low. You may experience bleeding after a shave biopsy. Your doctor may control it with a special ointment or a small electrical current that cauterizes the wound.
Punch biopsy: This is an incisional biopsy used to remove part of the lesion. It may be performed because the suspicious lesion is too large to be removed in its entirety, or if fully removing it would be disfiguring. To perform a punch biopsy, your doctor uses an instrument that looks like a cookie cutter to remove a skin sample. The device is rotated on the skin, cutting through all of its layers. After a sample is removed, your doctor will stitch the skin together.
“Optical biopsies”: Newer types of “virtual” biopsies can be done without needles, using a 3D imaging technique, called reflectance confocal microscopy, to capture images of suspicious lesions. This technology is both painless and non-invasive.
If you’re diagnosed with melanoma, your doctor may also perform some tests to determine whether the cancer has spread beyond the skin. The first place that melanomas usually spread is to nearby lymph nodes, so your doctor may feel under the arms, around your head and neck or in your groin area to determine whether any lymph nodes are enlarged. The doctor may also take a biopsy of suspicious lymph nodes.
Fine-needle aspiration (FNA) biopsy: The doctor uses a tiny syringe to remove small pieces of a lymph node or tumor and help determine whether the cancer has spread to nearby lymph nodes. Sometimes, imaging is needed to help guide the needle.
Surgical (excisional) lymph node biopsy: The surgeon is able to remove the entire enlarged lymph node through a small incision on the skin. This biopsy may be performed if the lymph node is large enough to suggest that the melanoma has spread, but an FNA biopsy didn’t find any cancer cells or wasn’t ordered.
Sentinel lymph node biopsy: The surgeon may perform a sentinel lymph node biopsy, in which a lymph node near the melanoma is removed and sent to the lab for further examination. This type of biopsy is often used when the melanoma has aggressive features that make it more likely to spread. This test is used to pinpoint the lymph nodes most likely to be affected. The procedure starts with a doctor injecting a small amount of a radioactive substance into the area around the melanoma and looking to see if it collects in one or more lymph nodes. The sentinel lymph node can be removed and examined. If there are no cancer cells in the lymph nodes, the cancer likely hasn’t spread, and no more lymph node surgery may be required.
There are certain key tests done on biopsy samples to help make a melanoma diagnosis, including:
Immunohistochemistry (IHC): This test uses antibodies to check for antigens or markers in the tissue sample that indicate the presence of cancer cells.
Fluorescence in situ hybridization (FISH): The FISH test can find specific changes in genetic material that may be associated with cancer.
Comparative genomic hybridization (CGH): This test looks at the genetic material or DNA in the tissue sample.
Gene expression profiling (GEP): The GEP test can find the root of and diagnose a disease and determine how well the body may respond to treatment. A melanoma biopsy may be tested for mutations in certain genes because this information can help guide treatment decisions.
Melanoma is more likely than other skin cancers to metastasize, or spread to distant bones or distant organs. Several medical imaging procedures, including a computed tomography (CT) scan, magnetic resonance imaging (MRI), positron emission tomography-computed tomography (PET-CT) scan or X-ray, may be used to detect cancer cells or tumors throughout the body. Patients with the earliest stages of melanoma typically don’t need these imaging tests since the disease likely hadn’t spread, according to the ACS.
Your doctor may suggest testing your biopsy sample to see whether the cells express changes in certain genes. For example, about half of skin melanomas show a mutation in the BRAF gene, according to the American Society of Clinical Oncology (ASCO). This information can help guide treatment decisions. Some newer drugs, such as BRAF inhibitors used to treat spreading melanomas, only work if the cells have BRAF mutations.
Besides BRAF, your melanoma biopsy sample may be tested for other genetic mutations, including:
Targeted drug therapies are being tested in clinical trials for these other genetic mutations as well. However, your melanoma may have another genetic change not yet identified, but know that researchers are trying to figure those out in clinical trials too. The good news is that care is becoming more personalized based on factors in cancer. Another gene test, DecisionDx-Melanoma, examines certain gene expression patterns in melanoma cells and can help you and your care team determine whether an early-stage melanoma is likely to spread or return, which can help further guide treatment options.
Learn more about diagnosing skin cancer
Next topic: How is melanoma treated?