For years, women with certain gene mutations or hereditary cancer syndromes have undergone prophylactic surgeries to reduce their chances of developing breast or ovarian cancer. Actress Angelina Jolie, perhaps the most high-profile example, chose to have a double mastectomy in 2013 and later had her ovaries and fallopian tubes removed after learning she carried a mutated BRCA1 gene. Jolie's mother died at 56 of ovarian cancer.
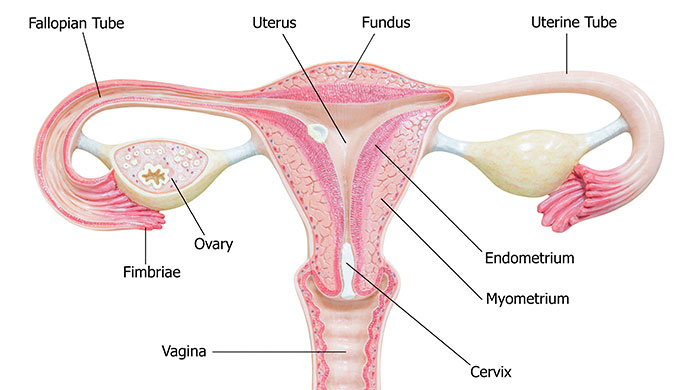
Now two prominent medical research and advocacy groups have issued updated guidance on who should consider surgical removal of the fallopian tubes, which lead from the ovaries to the uterus, to mitigate the risks of developing ovarian cancer.
“We’ve actually been following these recommendations for a few years now,” says Ruchi Garg, MD, Gynecologic Oncologist at City of Hope Atlanta. “If the patient is done having children and may be undergoing a tubal ligation, we recommend bilateral total salpingectomy, taking the opportunity to maximize the benefit. Additionally, if the patient is undergoing hysterectomy then standard practice for several years has been to remove bilateral tubes even if retaining the ovaries.”
With no reliable screening tests currently available for ovarian cancer, the updated recommendations suggest that most women, even those who don’t have genetic mutations known to predispose them to this cancer, should consider surgical removal of the fallopian tubes.
“Essentially, we want everyone with ovaries to know their risk level, and to know the actions they can take to help prevent ovarian cancer. Until there is a cure, these are our best weapons in this battle,” Audra Moran, President and CEO of Ovarian Cancer Research Alliance (OCRA), tells ocrahope.org. OCRA, along with the Society of Gynecologic Oncology developed and endorsed the new recommendations.
Research has shown that around 70 percent of the most common types of ovarian cancer begin as precursor lesions in the fallopian tubes and not in the ovaries. Moran says those who are done with childbearing should discuss with their doctors the possibility of having their tubes removed with a procedure called a salpingectomy, especially if they’re having any other pelvic surgeries.
This article will discuss:
- What prompted the latest recommendations?
- What are the risk factors for ovarian cancer?
- How can you assess your genetic risks
- Can I lower my risk?
- What should I know about having a salpingectomy procedure?
If you’ve been diagnosed with a gynecologic cancer and are interested in a second opinion on your diagnosis and treatment plan, call us or chat online with a member of our team.
What prompted the latest recommendations?
Ovarian cancer is the fifth-most common cancers among women in the United States, according to the American Cancer Society (ACS), and it accounts for more deaths than any other cancer of the female reproductive system.
Unlike cervical cancer, which may be identified early through a Pap smear, no such tests are available to screen for ovarian cancer. Being vigilant for symptoms is not always helpful, since ovarian cancer usually doesn’t cause symptoms until it’s progressed to more advanced stages.
However, a mounting body of research has established that many ovarian cancers originate in the fallopian tubes. This evidence prompted the most recent guidance on having them removed as an important risk-reducing procedure.
“There is a lot of good data behind [the new recommendations] showing that for folks who had [salpingectomy] surgery, the incidence rates of ovarian cancer are less,” Dr. Bill Dahut, ACS Chief Scientific Officer, told The New York Times. “If you look at the biology, maybe we should be calling it fallopian tube cancer and think of it differently, because that’s where it starts.”
What are the risk factors for ovarian cancer?
According to the ACS, “most women have one or more risk factors for ovarian cancer,” but the general population’s lifetime risk of developing the disease is less than 2 percent. This indicates that even common risk factors only slightly increase the chance of developing ovarian cancer.
Risk factors include those below.
Genetics: About 25-30 percent of women diagnosed with ovarian cancer have an inherited genetic mutation. In 20-25 percent of ovarian cancer patients, that mutation is in the BRCA1 or BRCA2 genes, which also are associated with breast cancer. Those with Lynch syndrome, an inherited condition, have a 12 percent risk of ovarian cancer. A family history of ovarian, breast, uterine, colorectal cancer also increases risk.
Acquired genetic mutations: Scientists have found that most genetic mutations associated with ovarian cancer are not inherited, but rather acquired through environmental factors. So far, though, they haven’t been able to pinpoint a specific chemical in our surroundings or food that can be connected to ovarian cancer, so more research is needed.
Endometriosis: This condition, is thought to be due to the lining of the uterus also known as the endometrium, growing outside the uterus. It can be associated with increased risk of ovarian cancer.
Age: Risks increase with age, with the highest risk among women between ages 55 and 64. Ovarian cancer is rare in women under age 40, and most cases occur after menopause, with half diagnosed in women ages 63 and older.
Hormone replacement therapy (HRT): Taking therapies with estrogen alone or combined with progesterone, especially for five or more years, may increase the risk.
Excess weight or obesity: Obesity, or a body mass index of 30 or more, also may reduce odds of survival in those diagnosed with ovarian cancer.
Reproductive history: Research has found a link between a higher number of menstrual cycles and the incidence of ovarian cancer. Your cancer risk may be increased if:
- You started menstruating at an early age
- Haven’t had children or had a first child after age 35
- Began menopause after age 50
- Experienced infertility
All of these circumstances may impact the number of menstrual cycles over the course of your lifetime.
How can you assess your genetic risks?
Since an inherited genetic mutation means a higher risk of ovarian cancer, genetic testing may help you assess your personal risk factors.
"Ovarian cancer is considered a rare disease, but for those with a family history and/or genetic mutation, the risk jumps to 40-50 percent or even higher,” says Moran. “So, knowing one's risk level is critical.”
To help individuals assess their genetic risks, OCRA has published a five-question survey to help you determine whether you’re eligible for free genetic testing the organization offers.
Even if you don’t qualify for OCRA’s free testing, you may want to talk to your doctor or seek out your own genetic counselor, especially if you have a family history of ovarian, breast, uterine, endometrial and/or colorectal cancers or are of Ashkenazi Jewish ancestry. Also, if you had genetic testing prior to 2013, ask your doctor or genetic counselor if you may need to be tested.
A genetic counselor is trained in assessing your risks based on family history and can discuss the pros and cons of genetic testing to establish whether you have a gene mutation that may increase the likelihood of developing ovarian cancer. A knowledgeable counselor can explain the results, and having this information may be helpful and even offer some relief from the stress and uncertainty of not knowing your inherited genetic risk.
As the OCRA notes: “Not all people with risk factors will get ovarian cancer. Some women who get the disease have no known risk factors, and most women with risk factors will not get ovarian cancer.”
Can I lower my risk?
The first step in mitigating your risk for developing ovarian cancer is to educate yourself. Pay attention to bodily changes that are not normal for you, especially if they last more than two weeks. Speak to your doctor about your individual circumstances and whether you notice any of these symptoms:
- Vaginal bleeding, especially if you’re past menopause
- Any unusual vaginal discharge
- Pelvic pressure or pain
- Abdominal or back pain
- Bloating
- Loss of appetite
- A change in bowel or urination habits like constipation or frequent urge to urinate
-
Oral contraceptives may decrease the risk of ovarian cancer
Your doctor may recommend a test like a rectovaginal pelvic exam, a transvaginal ultrasound or a CA-125 blood test to help confirm or rule out ovarian cancer.
Lifestyle factors that may reduce your risk include:
- Eating a healthy diet
- Getting regular exercise
- Maintaining a healthy weight
Patients undergoing a tubal ligation, a procedure used to cut and seal shut the fallopian tubes to prevent pregnancy, now are urged to consider either a partial or bilateral or complete salpingectomy or removal of both fallopian tubes, to mitigate ovarian cancer risks, Dr. Garg says. Those undergoing a hysterectomy—whether they decide to keep their ovaries or not—may also consider having their fallopian tubes removed at the same time. The procedure to remove the fallopian tubes is called bilateral salpingectomy and with additional removal of ovaries, it is called a bilateral salpingo-oophorectomy.
Some women decide to keep their ovaries because they produce beneficial hormones that have been linked to reducing risks of heart disease, osteoporosis and sexual dysfunction. Also, removing the ovaries would cause younger women to go into menopause early. For those at a heightened risk of ovarian cancer, doctors may recommend removing the ovaries along with the uterus and tubes or removing them in a later surgery. “There are several different combinations of surgeries that could be used to be able to maximize the benefits,” Dr. Garg says. “With careful surgery, if only the tubes are removed, the patient shouldn’t notice any effect beyond recovery from surgery because the tubes are not producing any hormones.”
What should I know about having salpingectomy?
Bilateral salpingectomy, removal of the tubes may be performed laparoscopically or through an abdominal incision, depending on the surgical procedure you undergo. The type of anesthetic used will depend on the type of surgery.
Laparoscopic surgery involves a small incision through which a narrow tube or robotic device with a light and camera attached is inserted to cut the fallopian tubes away from the uterus and ovary and cauterize and close the blood vessels. The procedure usually takes less than an hour and recovery time is typically two to four weeks.
If an abdominal incision is needed, the procedure may take longer and you may experience more discomfort around the incision site as you heal. Recovery time is usually about six weeks.
If you’re having just your fallopian tubes removed, you’ll continue to have monthly menstrual cycles. The eggs, however, won’t be able to move through the tube to the uterus, nor will sperm be able to fertilize the eggs, so you won’t be able to get pregnant.
Remember to talk to your doctor to help assess your risks for ovarian cancer. If you’re considering or scheduled for a pelvic surgery, explore the possibility of bilateral salpingectomy in addition to following the latest guidelines on mitigating ovarian cancer risks.
If you’ve been diagnosed with a gynecologic cancer and are interested in a second opinion on your diagnosis and treatment plan, call us or chat online with a member of our team.