Lettie Lassiter’s story is one of perseverance and survival. It’s also one of discovery. In 2013, Lassiter was diagnosed with stage 4 gallbladder cancer, news that devastated her and her family—and would soon get worse. By 2016, Lassiter’s cancer had spread to her brain, causing headaches and swelling and other symptoms, and the prognosis for a positive outcome was not good. But that was before Lassiter’s doctors discovered the gene mutations that were driving her cancer’s growth.
Lassiter’s story was highlighted in Part Two of Ken Burns Presents The Gene: An Intimate History, a two-night, four-hour documentary that aired on PBS on April 7 and April 14 and is now streaming on PBS.com. The Gene, adapted from the award-winning book of the same name by Dr. Siddhartha Mukherjee, tells the story of the rapid evolution of genetic science and the hope that the power to alter DNA will transform the treatment of some of the world’s most complex and challenging diseases, including cancer.
For Lassiter, who is being treated by doctors at Cancer Treatment Centers of America® (CTCA) in Atlanta, three rounds of chemotherapy showed early results, but her cancer continued to spread, and doctors were running out of treatment options. “I was down a lot,” Lassiter says in the documentary. “I had this cancer, and I have a husband and kids and grandkids, and I’m not going to be able to see them graduate and things like that.”
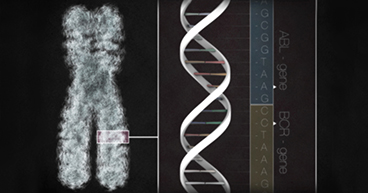
Her CTCA® care team ordered advanced genomic testing of Lassiter’s tumor, and it revealed multiple gene mutations, including some typically found in other cancers. Understanding how changes in her tumor cells fueled her cancer helped doctors identify a targeted therapy drug designed to attack that mutation.
“Knowledge of specific mutations within an individual cancer may make it possible to target that abnormality with the goal of interfering with the growth of the cancer and improving the survival of that particular patient,” says Maurie Markman, MD, President of Medicine and Science at CTCA.
The problem was that the U.S. Food and Drug Administration (FDA) had approved the targeted therapy to treat breast cancer, not gallbladder cancer. In 2017, Lassiter enrolled in the Targeted Agent and Profiling Utilization Registration (TAPUR) study, which gives participants access to drugs that have not been approved by the FDA for their cancer type. The TAPUR trial allowed Lassiter to take the breast cancer drug, which turned out to be instrumental in her progress.
“We were able to offer Lettie treatments that would not have been on the radar based on her disease type,” says Haritha Pabbathi, MD, Lassiter’s Medical Oncologist at CTCA Atlanta. “Genomic testing gave Lettie more treatment options.”
The Gene chronicles the story our understanding of genetics, from Gregor Mendel’s research in the 1800s to the emergence of CRISPR, the gene editing tool that may lead to precision treatments of complex diseases, such as cancer. Breakthroughs in genetics have led to the mapping of the human genome and to advanced genomic testing. The program also explores the ethical dilemmas that may arise with the ability to edit human DNA.
Gallbladder cancer is often difficult to diagnose in early stages because the disease may not cause symptoms. The five-year survival rate for a patient whose disease has spread, with occurs in more advanced stages, is as low as 2 percent. “With brain metastases, the prognosis becomes even worse—the average is less than six months,” Dr. Pabbathi says.
In the months after her new treatment, Lassiter’s tumors began to shrink, her symptoms had eased, and her quality of life improved. “This benefit of those treatments lasted for about two years, which is wonderful since most patients would normally not live that long,” Dr. Pabbathi says.
Lassiter’s disease has since progressed, and her treatment regimen has been changed, with her doctors continuing to look for ways to target the identified gene mutations. These treatments are considered palliative, meaning they are designed to ease symptoms and improve her quality of life, but they are not expected to kill her cancer entirely. Still, the power of precision medicine has helped Lassiter to feel better and allow her to spend more quality time with her family.
“I got my life back,” she says. “I feel like Lettie again.”