When long-time journalist Gwen Ifill passed away recently after a battle with endometrial cancer, her unexpected death cast an immediate spotlight on a disease that doesn’t get enough attention. A form of uterine cancer, endometrial cancer is the most common cancer of the female reproductive organs among U.S. women, according to the American Cancer Society (ACS)—yet much of the general public knows little about it. In the spirit of Ifill’s legendary career, spent breaking barriers for women in journalism and educating the public on important news of the day, our cancer experts wanted to take a moment to share key facts about endometrial cancer.
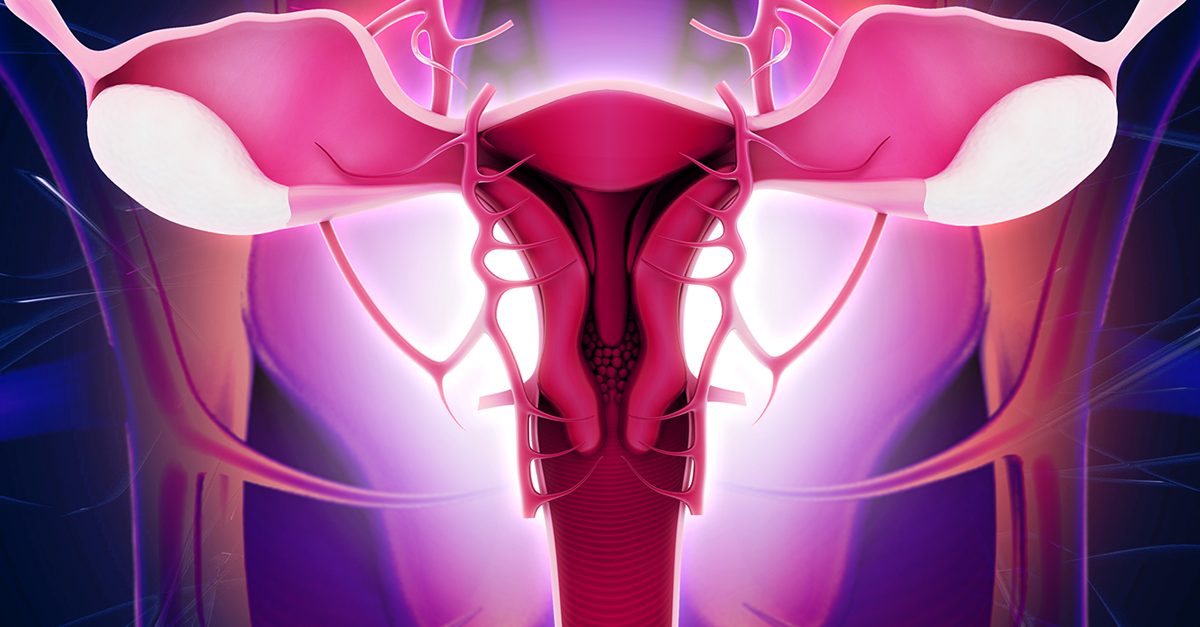
Endometrial cancer starts when cells in the inner lining of the uterus (endometrium) begin to grow out of control. Endometrial cancer and uterine cancer are sometimes used interchangeably, but uterine cancer is a broader term used to describe cancers affecting any area of the uterus, including but not only the endometrium. Another primary type of uterine cancer is uterine sarcoma, a rare tumor that forms in the muscle of the uterus. About 60,050 new cases of uterine cancer will be diagnosed in 2016 in the United States, according to the ACS. Typically, it’s one of the more treatable cancers—with five-year survival rates at 83 percent, the ACS estimates. More than 600,000 endometrial cancer survivors are living in the United States today.
Who gets endometrial cancer?
Endometrial cancer mainly affects postmenopausal women. The average age of women diagnosed with endometrial cancer is 60. While the disease is uncommon in women under the age of 45, rates of new cases in women younger than 50 have been climbing by just over 1 percent a year since 1988, the ACS reports. “We are seeing more endometrial cases in younger patients because of morbid obesity,” says Dr. John Geisler, Gynecologic Oncologist at our hospital near Atlanta.
Certain lifestyle factors increase a woman's risk for developing endometrial cancer, but they do not always cause the disease. Many women with one or more risk factors never develop endometrial cancer. “Obesity is the top risk factor,” says Dr. Geisler. “If you are 50 pounds overweight, you have a 10 times greater risk for endometrial cancer.”
Other risk factors for endometrial cancer include:
- Family history (having close relatives with endometrial or colorectal cancer)
- Changes in hormonal balance
- Diabetes
- A personal history with endometrial hyperplasia
- Past treatments with radiation therapy to the pelvis for another cancer
- No prior pregnancies
Can you screen for endometrial cancer?
There is no simple screening test for endometrial cancer. Cases of endometrial cancers are typically caught when women go to the doctor complaining of unusual spotting or bleeding. “After menopause, any vaginal bleeding is abnormal,” says Kelly Manahan, MD, FACOG,, Gynecologic Oncologist at our hospital outside Atlanta. “Any abnormal bleeding should be seen by a doctor, even if it’s just a small amount of bleeding or pink in color. Seeing a doctor may help lead to early detection.” A biopsy is typically performed on an endometrial tissue sample to test for cancer.
Other symptoms may include:
- Abnormal, non-bloody vaginal discharge
- Pelvic pain or cramping
- Unexplained weight loss
Endometrial cancer may be treated with a number of options, with the patient's age and overall health often factoring in as considerations. Treatment options include surgery, chemotherapy, hormone therapy and, in rare cases, radiation therapy. “Endometrial cancer is typically treatable if the correct treatment is used,” says Dr. Manahan. “The bottom line is any abnormal spotting or bleeding should be seen by a doctor.”