

This page was reviewed under our medical and editorial policy by
Peter Baik, DO, Thoracic Surgeon
This page was updated on January 8, 2023.
To determine a lung cancer diagnosis, the care team uses tests and tools designed for diagnosing and evaluating the disease so they can develop an individualized treatment plan.
For example, imaging and laboratory tests are used to track the size of the tumor(s), monitor the patient's response to treatment, and modify that plan when needed.
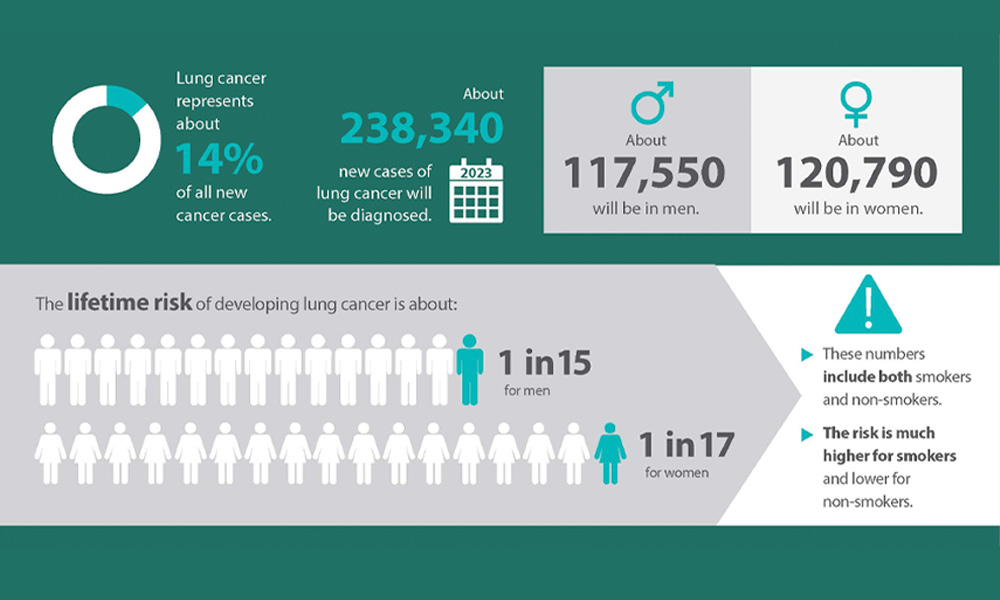
Download lung cancer infographic »
The lung cancer team may use imaging tests to look inside the patient's lungs and chest. There are a number of different imaging tests, including:
These imaging tests may be used to:
A chest X-ray uses high-energy electromagnetic radiation to provide images of the lungs and surrounding tissues.
A normal chest X-ray allows the care team to visualize the lungs, heart, bones and other structures, but it doesn't help identify cellular abnormalities. Abnormal chest X-rays may reveal issues such as shaded areas, which may be evaluated further to determine whether they’re lung nodules or tumors.
A CT scan reveals the anatomy of the lungs and surrounding tissues, which may show tumors more clearly than an X-ray would, although the CT scan wouldn't indicate whether tumors are cancerous. The care team uses CT scans to diagnose and monitor tumor growth.
A CT scanner takes a series of X-rays from different angles, processes them using a computer and produces cross-sectional views of the patient's body. CT scans can reveal lung tumors—their size, shape and position—as well as show whether the cancer has potentially spread to the patient's lymph nodes, adrenal glands, liver or other organs.
If neurological symptoms have developed, a CT scan of the brain may be performed to check for metastasis if the patient cannot receive an MRI scan.
If the patient is experiencing shortness of breath, the radiologist may perform a CT angiogram to check for blood clots or other blockages in the lungs.
The U.S. Preventive Services Task Force recommends that patients undergo a low-dose CT scan each year if they meet all of the following criteria:
This type of CT scan uses a very low dose of radiation to make detailed images of the lungs. It is safe and causes no pain. Radiation from a low-dose CT scan is similar to the amount the patient would get from six months of natural background radiation, whereas a regular-dose CT scan of the chest compares to two years of natural background radiation.
Using radio waves and strong magnets, MRI is used to look for lung cancer spread to the brain or spinal cord. It may also be used to evaluate for invasion into surrounding structures.
A PET scan involves injecting the patient with a special radioactive tracer that collects in areas with high tracer uptake. Most cancer cells have high activity and show up as bright spots on PET scans.
A PET/CT scan is a nuclear imaging technique that combines CT scan technology with positron emission tomography into one machine. A PET/CT scan shows both the structure and increased metabolic activity of cells and tissues in the body during a single imaging session. In the case of lung cancer, this scan provides a more comprehensive view of the body to determine the presence of abnormal activity, even before a tumor may have developed.
Combining PET/CT technology enables the care team to know the extent of the disease and whether it has spread to other parts of the body. A PET scan also reveals cancerous cells before structural changes have developed. This approach helps pinpoint tumors, so that the care team may properly diagnose and stage the disease, and focus treatment on the cancerous tissues.
If imaging tests suggest the possibility of lung cancer, the care team may want to examine cells from the patient's lungs under a microscope in a lab to help confirm the diagnosis.
Lung cells can come from:
Doctors may wish to look at a sample of the patient's sputum if they suspect lung cancer that started in the major airways of the lung, such as squamous cell lung cancer. The patient is asked to provide samples by coughing up mucus in the morning for three consecutive days.
If the patient has fluid building up around his or her lungs, the care team may wish to study it to determine whether the patient has cancer of the lining of the lungs, between the lung and chest wall. (Fluid buildup around the lung also can be caused by heart failure or an infection.)
To remove a sample, doctors numb the skin before inserting a hollow needle between the ribs. The needle removes fluid that is then sent to a lab. The lab looks to see whether the fluid contains malignant (cancerous) cells.
During a lung biopsy procedure, the doctor removes a small piece of tissue or fluid from the chest so it can be checked for cancer cells.
Biopsies may be performed with needles or through a surgical incision. One advantage to using a needle is that it can be done through the skin or the airway and does not require surgery. However, needle biopsies remove only a small amount of tissue. This small amount of tissue may not provide enough information to diagnose cancer and to perform genomic tests.
Biopsies for lung cancer involving needles include:
The doctor will use a syringe that has a very thin, hollow needle to remove cells and tiny fragments of tissue from suspicious areas. An FNA is often performed to look for cancer cells in the lymph nodes between the lungs.
The doctor may use a larger needle to remove a larger sample of tissue from the patient's airways. This procedure is called a core biopsy because the tissue that’s sampled is a small core. The larger sample size is an advantage of having a core biopsy.
This type of biopsy may be performed if the care team suspects a tumor is located in the outer part of the patient's lungs. During a transthoracic needle biopsy, a needle is inserted through the skin of the chest wall. The patient is given local anesthesia to numb the area. The doctor uses a type of X-ray known as fluoroscopy or a CT scan to help guide the needle.
A transthoracic needle biopsy may allow air to leak out of the lung and into the space between it and the chest wall. This is called a pneumothorax, and it describes partial or complete collapse of the lung due to air being trapped between the lung and the chest wall.
If the leak is tiny, it should get better on its own without treatment. If the leak is large, doctors will insert a chest tube into the space to suck out the air. It could take a day or two to stop. The tube is removed once the risk of lung collapse disappears.
The care team may use a bronchoscopy to look for tumors or blockages in the larger airways of the patient's lungs. A bronchoscopy involves putting a bronchoscope, a thin flexible tube with a light and a video camera, down the patient's throat and into his or her airways. Various procedures can be performed through a bronchoscope.
Below are different types of bronchoscopy the doctor may order.
This technology allows physicians to identify cancerous cells in the bronchial tubes that may not be visible under white light examination. The doctor can then remove a small sample of abnormal tissue for further analysis.
A navigational bronchoscopy combines advanced imaging techniques with electromagnetic navigation to help find and treat cancer in the lungs. This procedure allows doctors to reach tumors by advancing the scope into smaller bronchi or bronchi that are blocked by a tumor.
For patients for whom an area of concern cannot be reached via traditional, navigational bronchoscopy, robotic bronchoscopy may be an option. Robotic bronchoscopy may help certain patients avoid a transthoracic needle aspiration, which may increase the risk of complications. Robotic bronchoscopy is also designed to increase the chance of a successful biopsy.
A transtracheal FNA or transbronchial FNA may be performed during a bronchoscopy or an endobronchial ultrasound.
An endobronchial ultrasound is performed by inserting a flexible scope through the mouth into the larger airways and using ultrasound waves to image the tissue.
After a patient is diagnosed with lung cancer, it’s important for the treatment team to know whether it’s solely in the lungs or it’s spread to the lymph nodes or other organs. When cancer spreads, it's known as metastasis.
Below are tests that can help identify lung cancer spread.
EBUS is a less invasive bronchoscopic procedure used to evaluate and sample cancerous cells in the chest. In most cases, EBUS is performed as an alternative to a mediastinoscopy, a surgical procedure used to collect samples in the chest while the patient is under general anesthesia.
With this ultrasound, doctors insert an endoscopic ultrasound device into the esophagus to see whether nearby lymph nodes contain lung cancer cells.
Both of these tests are used to look more closely at the lymph nodes along the patient's windpipe and bronchial tubes. Which procedure the doctor recommends depends on where the suspected spread is and how big a sample is needed.
With a mediastinoscopy, a lighted tube is placed behind the breastbone to help look around and take samples to be analyzed in a lab. A mediastinotomy may be needed if certain lymph nodes can’t be reached with the mediastinoscopy procedure. A mediastinotomy requires an incision (roughly 2 inches long) be made between the second and third ribs on the patient's left side. This procedure allows the doctor to also look around and collect samples for analysis.
The care team may order a thoracoscopy to determine whether the lung cancer has invaded the space between the lungs and chest wall or the lining of these spaces. The doctor will use a thoracoscope—a thin, flexible tube that has a light and a tiny video camera on the end of it—to see inside the chest. The tube is inserted through a small incision that is made between the ribs and the bottom of the patient's shoulder blade.
Thoracoscopy also may be used in some cases as a treatment for early-stage lung cancer. The part of the lung where the cancer is located may be removed using this procedure.
The care team also may order the following tests to aid in diagnosis and determine the patient's individual treatment plan.
Currently, no blood test can detect lung cancer. However, blood tests may be used to help determine the patient's overall health and whether he or she is able to undergo surgery if that is part of the treatment plan. Blood tests that the doctor may order include:
Complete blood count (CBC): A CBC blood test looks at a number of different types of blood cells. The patient's red blood cell count can indicate whether he or she has anemia; the count would be low. A low number of platelets could suggest that the patient might have trouble with bleeding. Low white blood cell counts could suggest that the patient is at risk of infections. The care team may order a CBC several times during treatment, especially if the patient has been given cancer drugs, as these may affect bone marrow, which is where blood cells form.
Other blood chemistry tests: Lung cancer may spread to other organs, such as the liver, kidneys or bones. The care team may order different blood tests that can indicate whether the lung cancer has spread to these sites. An example: A higher-than-normal level of calcium and alkaline phosphatase may indicate that lung cancer has metastasized to the bone.
Liquid biopsies: In the fall of 2020, the U.S. Food and Drug Administration approved two blood tests—Guardant360 CDx® and FoundationOne Liquid CDx®—that may be used to look for genetic changes in a tumor that may help guide treatment. Known as liquid biopsies, both were approved for non-small cell lung cancer. Guardant360 CDx® looks for changes in more than 60 genes, while FoundationOne Liquid CDx® looks for changes in more than 300 genes. The genetic changes that are detected may then be matched to available drugs and help personalize the patient's treatment.
Lung cancer genomic testing: Advanced genomic testing examines a tumor on a genetic level to look for the DNA alterations that are driving the cancer’s growth. By identifying the mutations that occur in a cancer cell’s genome, we can better understand what caused the tumor and tailor treatment based on the findings from the test. The most common tumor markers tested for in lung cancers are EGRF, KRAS and ALK.
Nutrition panel: With this test, the care team evaluates patients for deficiency of nutrients, such as vitamin D and iron. The test helps the care team identify the nutrients patients need replaced or boosted to support their quality of life.
If you’re interested in scheduling an appointment with our rapid lung-nodule diagnosis program, call us or chat online with a member of our team.Next topic: How is lung cancer treated?