It can be unsettling to find signs of blood in your stool. But you shouldn’t immediately think the worst. True, blood in the stool may be caused by a variety of health conditions or diseases, including cancer, that could develop into serious health issues if left untreated. But the blood may also be a product of more benign conditions, such as hemorrhoids, which, while still unwanted, are often less serious than other conditions.
Still, if you notice blood in your stool after a bowel movement or blood when wiping, it’s a good idea to contact your doctor to find the cause, says Toufic Kachaamy, MD, Chief of Medicine at City of Hope Phoenix.
“Blood in the stool is always abnormal and needs to be investigated,” he says. “Never assume it’s benign or not significant until you’ve had a thorough investigation by your physician.”
In this article, we’ll explore the causes of rectal bleeding and bloody stools and what you should do about them, as well as explaining when to worry about blood in stool. Topics include:
- Conditions that may cause blood in stool
- Symptoms that may accompany rectal bleeding
- Rectal bleeding and cancer
- Why the color of the blood matters
- Rectal bleeding in young adults
If you’ve been diagnosed with cancer of the digestive system, including colorectal cancer, stomach cancer or esophageal cancer, and are interested in a second opinion on your diagnosis and treatment plan, call us or chat online with a member of our team.
Conditions that may cause blood in stool
Your poop is made up of about 75 percent water, but it also contains an amalgam of undigested bits of food, mucus, dead cells and bacteria.
What shouldn’t be in your poop? Blood.
Many conditions, including cancer, that cause blood to appear in your stool may become serious if not addressed early. Some are related to auto-immune conditions, caused when an overactive immune system attacks healthy cells in the body. Others develop over time, perhaps due to diet or lifestyle, and may cause only minor pain or discomfort.
Conditions, other than cancer, that may cause blood in stool include:
Anal fissures: Small tears in the lining of the anus may be caused by constipation, difficult bowel movements or sexual activity.
Crohn’s disease or colitis: These auto-immune conditions may cause inflammation of the digestive system, leading to diarrhea and abdominal pain.
Diarrhea: Runny stools caused by illness, contaminated food or overindulgences may result in a sore or inflamed anus and blood streaks that appear on toilet paper after multiple bathroom trips.
Food poisoning: Tainted food may lead to infections that cause severe digestive distress.
Diverticulosis: Pouches in the lining of the colon, called diverticula, may become inflamed or infected.
Hemorrhoids: Swollen blood vessels in the rectum or on the anus may develop due to constipation or frequent sitting.
Ulcers: Open sores in the lining of the stomach or bowels are often caused by a bacterial infection.
Some of these conditions may heal or resolve themselves within a few days. But if they produce blood in the stool at any time, you should still tell your doctor, Dr. Kachaamy says.
“Sometimes blood in the stool can be caused by benign conditions such as hemorrhoids, a small fissure after constipation or an infection and can resolve on its own,” he says. “However, bleeding from cancer or inflammatory bowel disease can also be intermittent, and so any bleeding needs to be investigated.”
Symptoms that may accompany rectal bleeding
In addition to bleeding, other symptoms may develop from some of these conditions. It’s important to tell your doctor about all the symptoms you’ve been experiencing and any family or personal history that may be related to your condition.
Other symptoms may include:
- Itching or burning in the anus
- Diarrhea or constipation
- Nausea or vomiting
- Cramps
- Bloating
- Pain
- Fever
Rectal bleeding and cancer
Blood in the stool often is a sign of bleeding in some area of the digestive tract, from the esophagus to the anus. And while bleeding may occur for a number of reasons, including the conditions listed above, it’s important to either rule out cancer or catch it when signs appear.
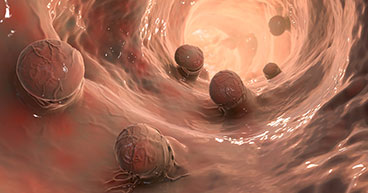
Cancer develops when mutated or damaged cells grow out of control. In many cases, the damage has affected the systems in the cells that regulate their growth and division. Cancers in the digestive system often develop in the soft lining of the esophagus, stomach, bowels or rectum and typically cause inflammation and bleeding.
Why the color of the blood matters
The color of the blood and the texture of the bloody stool may be influenced by many factors, especially what you’ve eaten. Beets can produce stool that turns the toilet water red or purple, while green, leafy vegetables rich in chlorophyll may produce darker stools.
If the bloody stool was caused by diseases such as cancer, the stool color may indicate where the bleeding is coming from in the digestive tract and may help doctors find its source.
For instance:
- Bright red blood in stool often means the blood is fresh and the bleeding is lower in the colon or rectum. This condition is called hematochezia.
- Dark red blood may mean the bleeding is higher in the colon or in the small intestine.
- Dark, tarry stool may mean the bleeding is in the stomach or the gastroesophageal junction—where the stomach meets the esophagus. This condition is called melena.
Polyps, which are small growths in the lining of the colon, may also grow and begin to bleed. Polyps may be benign at first, but they may develop into cancer. That’s why it’s important to talk to your doctor about when to get a colonoscopy, which is considered the gold standard for detecting colorectal cancer early. Colon polyps found during the procedure may be removed during the colonoscopy.
Rectal bleeding in young adults
While cancer is most commonly diagnosed in older adults, young adults often develop conditions that may cause rectal bleeding. Irritable bowel diseases such as ulcerative colitis or Crohn’s disease often first begin affecting adults in their 20s or 30. These conditions may increase the risk of colorectal cancer later in life.
Also, new diagnoses of colorectal cancer are surging in young adults. The disease is now the leading cause of cancer deaths in people 20 to 45 years old. Dr. Kachaamy says young adults should not ignore blood in the stool, even if it goes away after a few days.
“While some conditions that cause bleeding resolve themselves quickly without treatment, other conditions like cancer and inflammatory disease will need treatment. Identifying them early offers you a stronger change for a better outcome,” he says. “Colorectal cancer—especially rectal cancer—is on the rise in young adults, and we currently do not screen average-risk adults below the age of 45. This means that to diagnose these diseases early, you need to be vigilant to early symptoms such as bleeding and not neglect these symptoms.”
If you’ve been diagnosed with cancer of the digestive system, including colorectal cancer, stomach cancer or esophageal cancer, and are interested in a second opinion on your diagnosis and treatment plan, call us or chat online with a member of our team.